COMPLETE TAVR: Where are we in 2025?
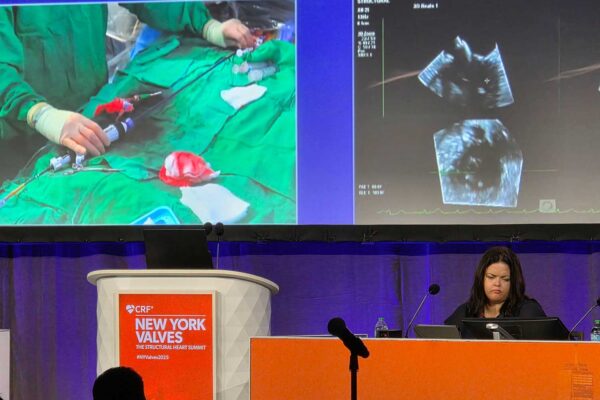
The New York Valves Structural Heart Summit, which took place between June 24-27, brought together thousands of the world’s leading cardiologists in an annual gathering to discuss the latest advances in the diagnosis and treatment of structural and valvular heart disease. This year, a spotlight was placed on the topic of how to best manage patients with severe aortic stenosis and concomitant coronary artery disease. Should these patients undergo revascularization, and if so, when is the right time to perform it?
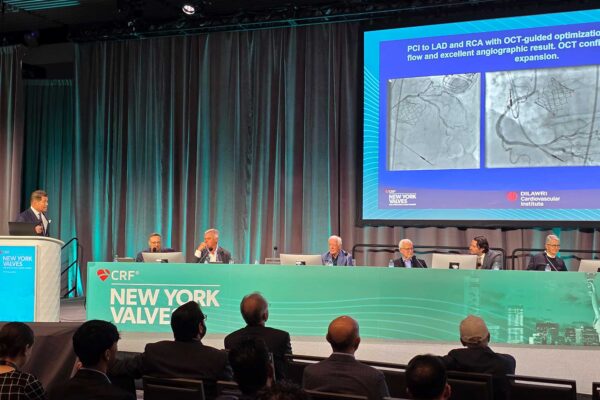
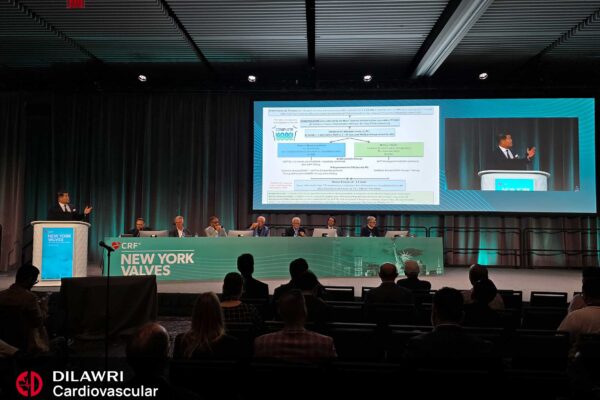
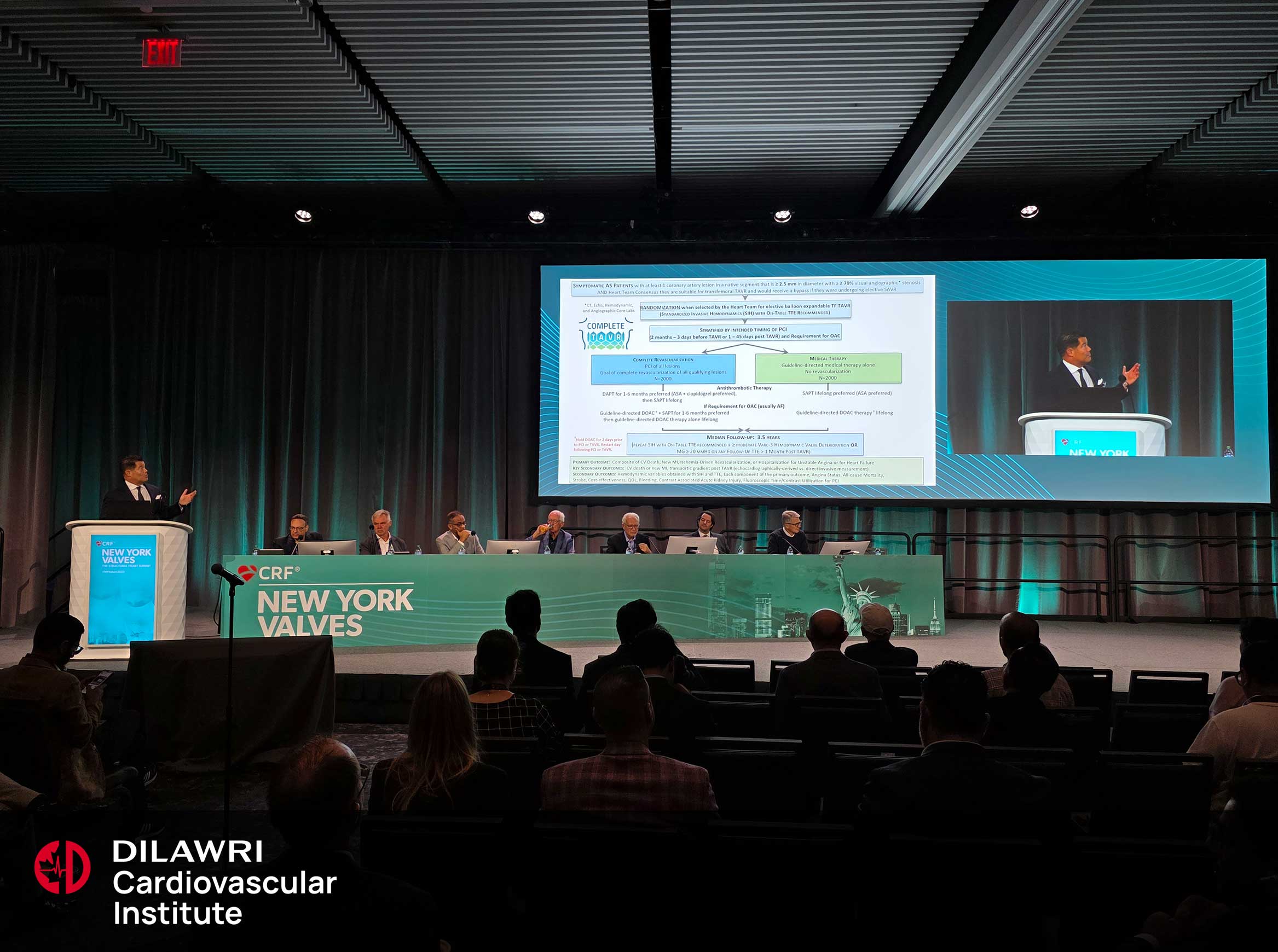
Some of these questions are being explored in the COMPLETE TAVR trial, now the world’s largest multi-centre randomized clinical study that aims to definitively answer the question of whether complete revascularization or medical therapy alone is more effective at reducing the composite outcome of adverse cardiovascular events in this population. Since its initiation in 2020, the trial, led by Dilawri Cardiovascular Institute (DCI) investigator, Dr. David Wood, has enrolled more than 600 patients with over 75 participating research sites across the globe. Target enrollment is expected to reach the thousands by the end of the next 3.5 years.
Coronary artery disease: to treat or not to treat?
Over time, the number of TAVRs performed in younger patients who fall into the lower risk category has increased. For the right patient, a transcatheter approach can have advantages over surgery, including potentially a reduced risk of complications such as stroke and valve thrombosis, as well as a much shorter recovery time.
If a patient also has coronary artery disease, clinicians also need to pay attention to the timing of revascularization, which could have an impact on overall procedural risks and patient outcomes. Performing TAVR before revascularization could impede access to coronary arteries needing imminent or future intervention and increase the risk of hemodynamic instability provoked by untreated coronary artery disease. However, revascularization prior to TAVR may increase the risk of bleeding complications and require patients to be on extended dual antiplatelet therapy. The movement in the last several years seems to be towards a more conservative approach to revascularization, but signals in both directions highlight the value of large-scale data from a trial such as COMPLETE TAVR.
The need for definitive answers
The goal of COMPLETE TAVR is to provide prescriptive guidance on the management of patients with aortic stenosis and coronary artery disease, but it’s not the first study to explore the complexities of treating this patient population. One meta-analysis conducted by Lateef and colleagues in 2019 showed that there were no differences in 30-day or 1-year all-cause mortality between TAVR and TAVR with PCI (percutaneous coronary intervention). In 2021, the ACTIVATION TRIAL compared PCI to no PCI prior to TAVR and found that there was no difference in the risk of death or rehospitalization at 1-year, and that there was an increase in bleeding events in patients who did receive PCI.
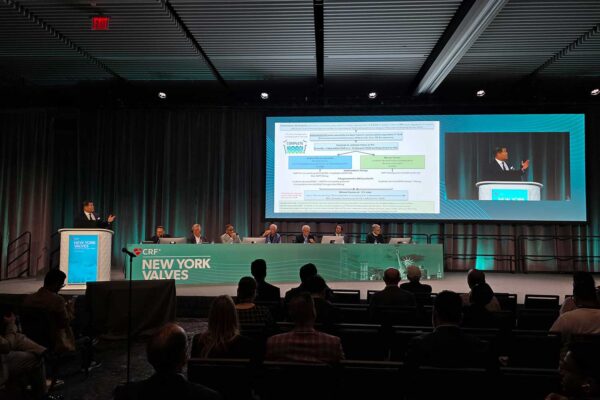
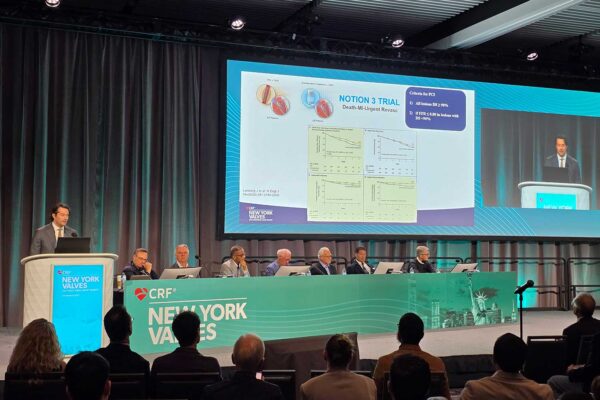
The NOTION 3 trial, which was published in 2024 and enrolled approximately 500 patients, compared TAVR with PCI to TAVR with medical therapy alone. The criteria for PCI were that treated lesions needed to be >90% or have an FFR ≤0.80 if <90%. Research found no significant difference in mortality but did observe improvements in the TAVR with PCI arm when it came to unplanned revascularization and myocardial infarction, albeit with an increased bleeding risk at 1-year. Notably, patients with clinically significant lesions (i.e., >90%) benefitted the most from revascularization, providing further support for the selective treatment of symptom-inducing or ischemically-driven disease.
In addition to these studies, there are two notable ongoing trials, the TAVI-PCI trial, which focuses on the timing of PCI and the FAITAVI trial, which takes a closer look at the role of ischemia in the decision to revascularize. The key takeaway is that although studies have been, and continue to be conducted, none have reached the scale or richness of data of COMPLETE TAVR.
Equipoise in action
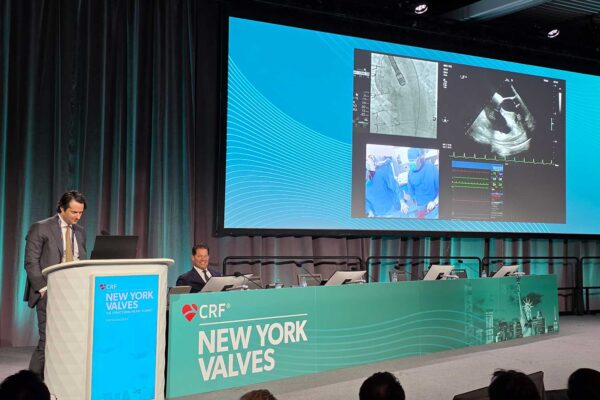
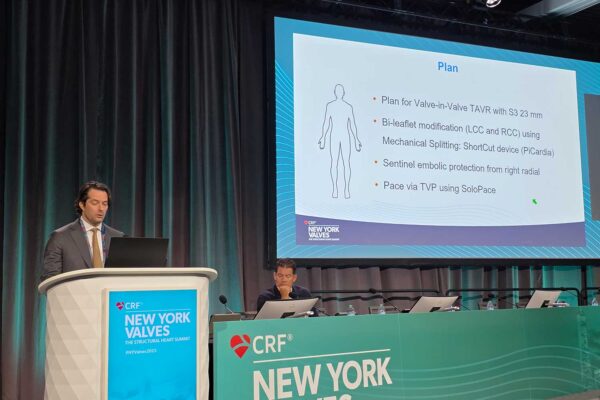
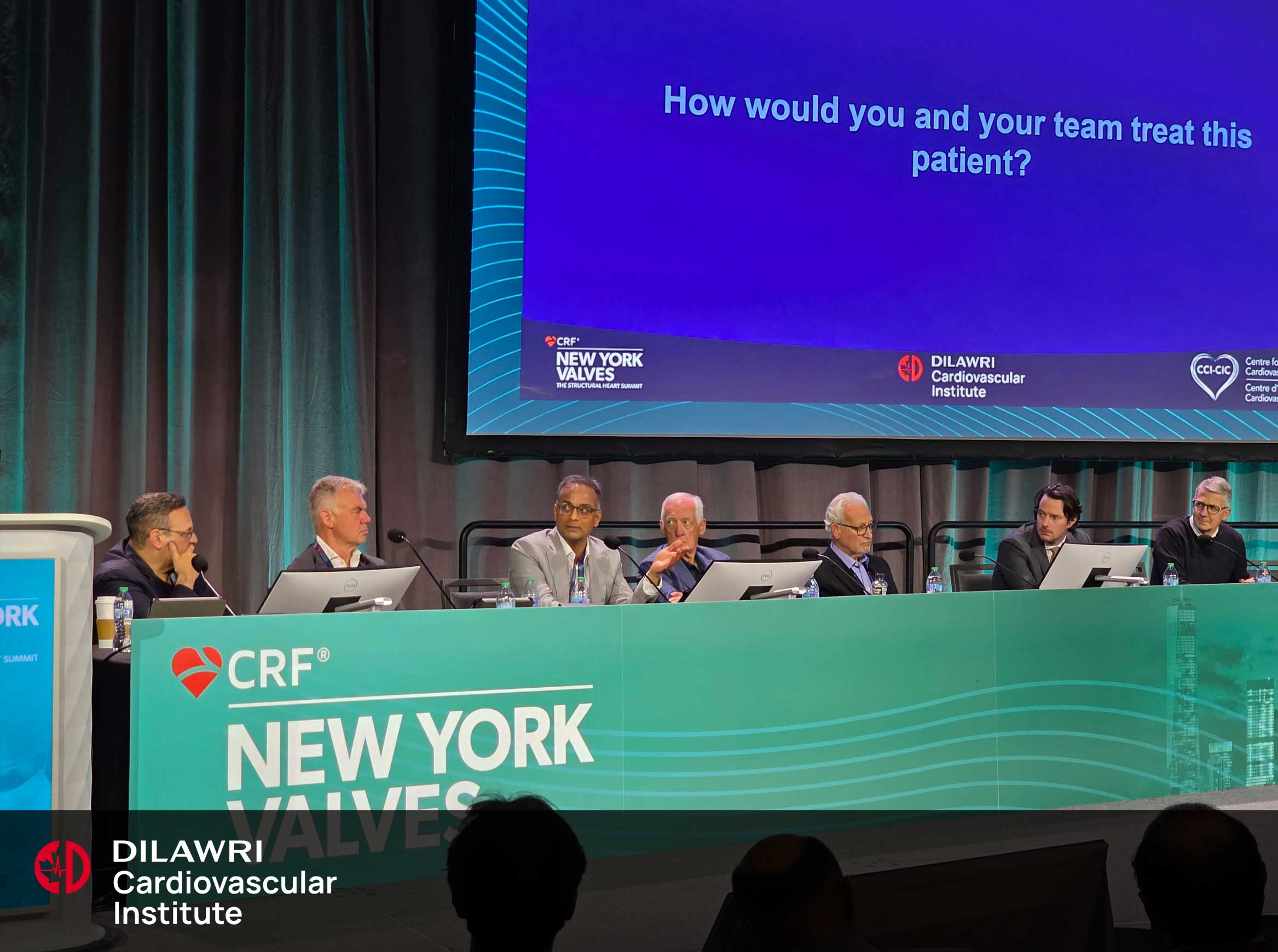
The variation in treatment strategies became apparent during a panel discussion in which DCI presented three of its own cases that exemplified equipoise. Panel members Dr. Michael Mack, Dr. Tej Seth, Dr. Philippe Genereux, Dr. Stephan Windecker, Dr. Martin Leon, Dr. Dave Cohen, and Dr. John Webb were invited to weigh-in on how they would approach proximal, complex and multivessel cases. Factors such as whether a patient was experiencing both dyspnea and angina, coronary anatomy, and the presence or absence of atrial fibrillation were identified as being important to a heart team’s treatment planning. Also discussed was the care that should be taken when framing the risks for patients and honouring patient choice.
In response to the first case presented, Dr. Cohen offered that “there is no compunction to do PCI in a patient [who has had their aortic stenosis treated]. It may be convenient to do it, […] but you are not saving the patient’s life by doing a PCI on the LAD.” It’s a controversial opinion, but treating the aortic stenosis first can, in some cases, provide complete symptom relief and eliminate the need for another procedure. So, while guidelines exist for how certain subsets of coronary artery disease should be treated, in the context of symptomatic aortic disease, it’s important for clinicians to continuously weigh the potential risks and benefits. Clinically significant coronary disease may be present but may not be prognostically significant.
The importance of continued enrollment
Reflecting on the significance of the COMPLETE-TAVR trial, Dr. Stephan Windecker offered some thoughts: “I really think this is a very timely study and we need a definitive answer. Our notion of the […] prognostic impact of coronary artery disease has swung into a very conservative direction [and] therefore, I think this trial is exceedingly important.”
Dr. Michael Mack echoed these sentiments, saying that “The pendulum has swung over the last 10-20 years from complete revascularization to ‘leave it all alone it’s bystander disease’ and I think the pendulum has probably swung too far that way. I don’t think the results of this trial, no matter which way it is, is a definitive yes-no. The key is going to be in all the analysis of the subgroups, because the disease is so nuanced, there’s not a yes-no dichotomous answer here.”
The findings of the COMPLETE TAVR trial are expected to strongly influence global coronary, transcatheter, and surgical guidelines and give rise to numerous future sub studies, including those focused on coronary access antithrombotic therapies, stenosis severity, lesion location, intracoronary imaging, CT FFR, quality of life, and cost effectiveness. In their closing remarks, Dr. Wood and panelists stressed the importance of continuing to enroll into the trial and encouraged interested research sites to become involved.
”“We all see patients every day that have both aortic valve and coronary artery disease. We must work together to answer this crucial question. The results will change global practice."
Dr. David Wood